Gastroesophageal reflux disease (GERD) in children is a digestive disorder in which the gastric acid from the stomach moves upward into the esophagus. Most people have gastric acid reflux occasionally, however, if reflux is occurring frequently, it can develop into GERD.
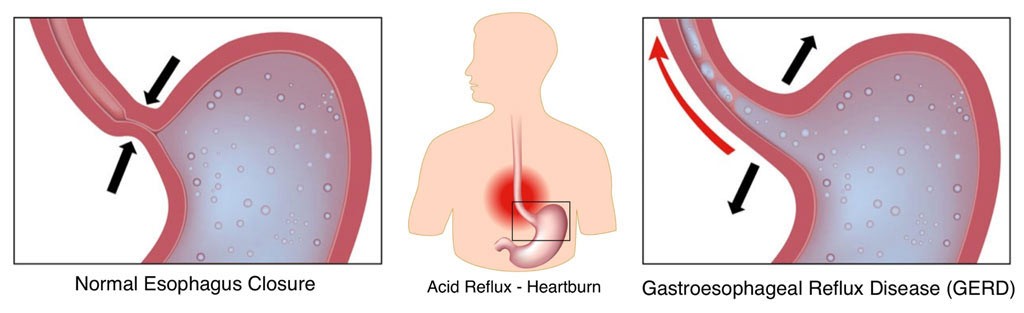
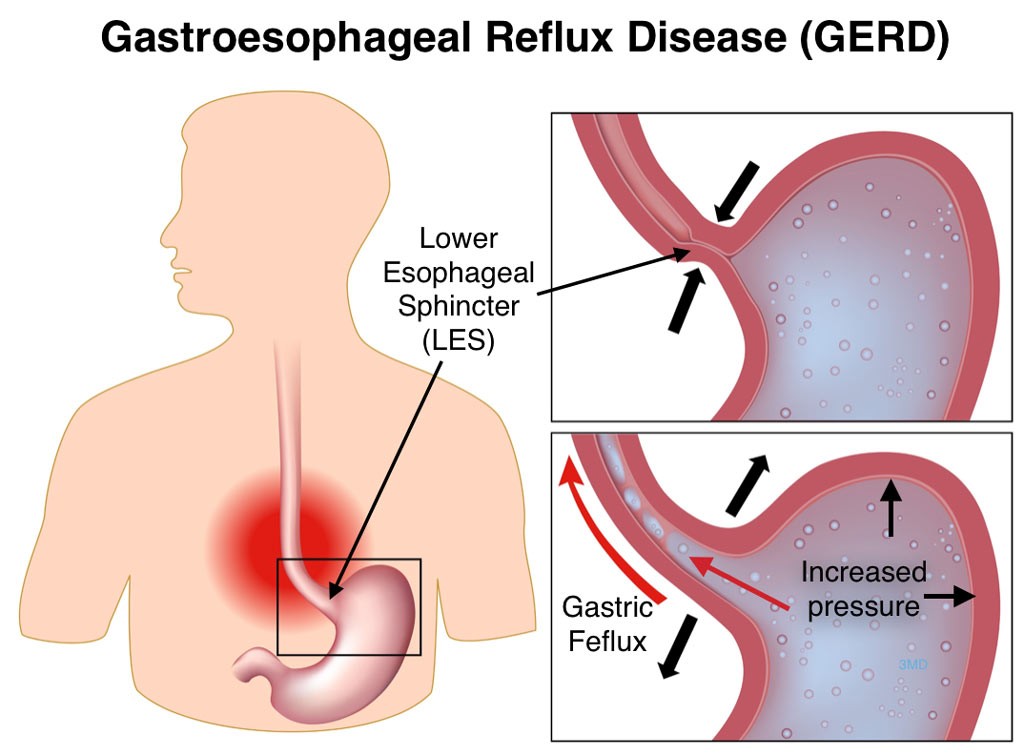
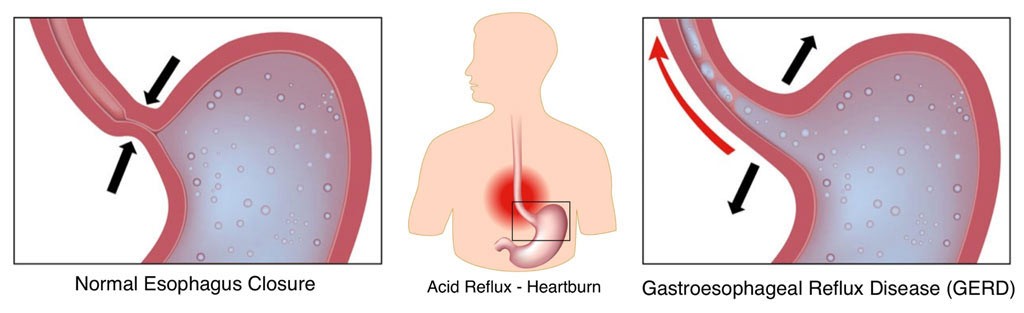
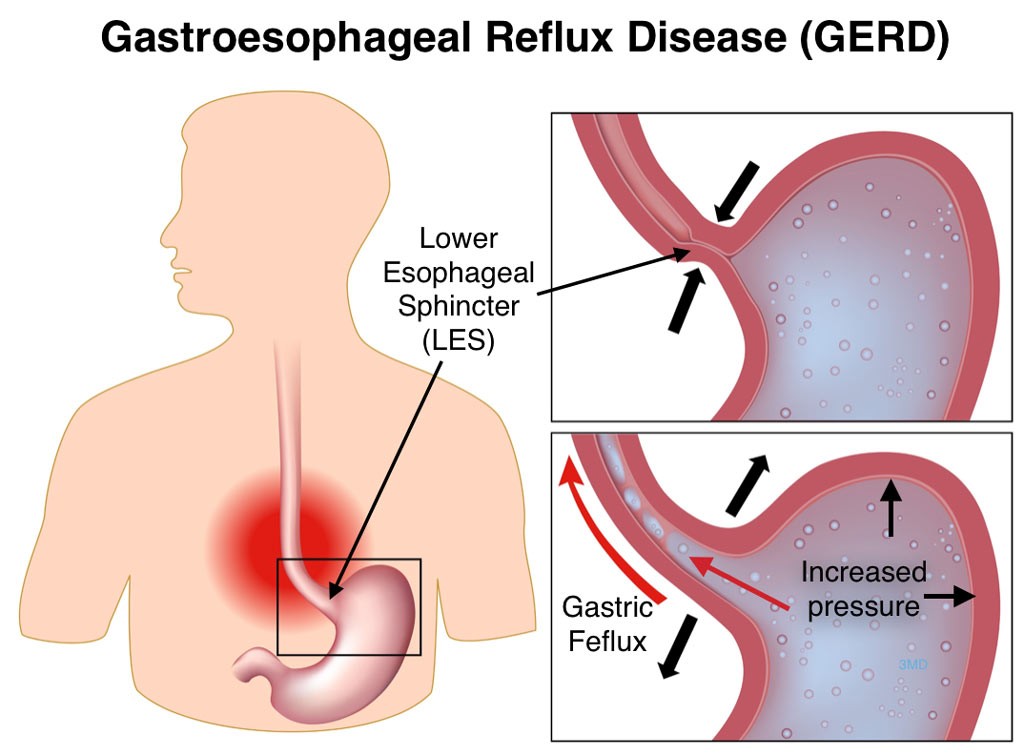
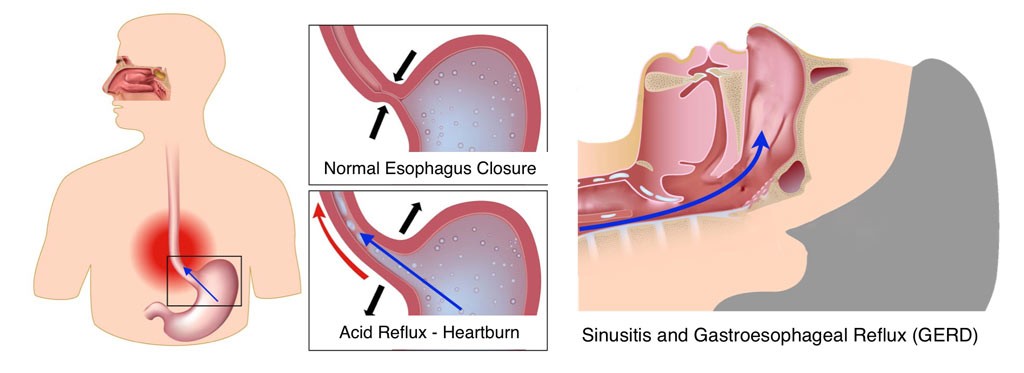
Gastroesophageal reflux (GER) is the result of a malfunctioning valve at the end of the esophagus. This lower esophageal sphincter (LES) muscle normally opens and closes to allow food into the stomach. If the muscle opens, or relaxes, longer or more often than it should, stomach acid refluxes into the esophagus. This reflux can cause heartburn or vomiting. If reflux enters the throat, trachea (wind pipe) it is referred to as laryngopharyngeal reflux, which results in throat clearing, throat pain, coughing and chest congestion.
GER is a common occurrence in infants, with more than 50% of children 3 months or younger having at least one vomiting episode per day. The majority of babies outgrow GER by age 1 due to increased muscle control.
Older children who are experiencing GER need to be evaluated by a doctor to determine the cause of the problem and receive treatment.
Symptoms of Gastroesophageal Reflux Disease (GERD) in Children
Heartburn is the most common symptom of GERD in adults, but children may or may not experience heartburn. When they do, they often have difficulty describing the sensation. Children with GERD typically complain of tummy pain or chest discomfort, most frequently after meals. Common symptoms of GERD include digestive and pulmonary symptoms:
- Heartburn
- Frequent vomiting
- Excessive burping
- Refusal to eat or gagging during eating
- Weight loss
- Poor appetite
- Bad breathe (halitosis)
- Cavities or breakdown of tooth enamel
- Choking sensation
- Persistent cough or throat clearing – caused by secretions of the larynx (voice box)
- Sore throat, pain with swallowing (dysphagia) – caused by recurrent tonsil infection
- Hoarseness (dysphonia)
- Breathing problems, wheezing or congestion
- Croup – (laryngotracheitis )
- Frequent upper respiratory or ear infections
- Ear pain (otalgia)
Causes of Gastroesophageal Reflux Disease (GERD) in Children
GERD
Causes of GERD in children are typically different than the causes for infants or adults. Anything that increases pressure below the lower esophageal sphincter (LES) can contribute to a child having GERD, including:
- Overeating
- Obesity
- Constipation
- Medication: Some antihistamines, pain medicines and antidepressants can contribute.
- Second-hand smoke
- Certain foods that can affect the functionality of the LES can be a factor in GER:
- Peppermint
- Foods high in fat
- Acidic foods, such as citrus (lemons, limes, oranges), tomatoes and tomato sauces
- Chocolate
- Carbonated beverages and caffeine
Diagnosing Gastroesophageal Reflux Disease (GERD) in Children
Diagnosing GERD in a child can usually be done by a physical examination of the child and interviewing the child’s caregiver. In some instances, further testing may be recommended. These include:
- pH probe and impedance testing: A thin tube with a sensor at the end is inserted through the nose to the bottom of the esophagus. While in place (usually 12-24 hours), the sensor measures how often and how much acid is refluxed from the stomach to the esophagus.
- Upper GI series (barium swallow): The child swallows barium (a white, chalky liquid) and a video x-ray machine tracks the barium through the esophagus, stomach, and upper intestinal tract to detect any obstructions, abnormalities, or narrowing which could cause the reflux.
- Upper GI endoscopy: An ultra-thin, flexible tube equipped with lights and camera (endoscope) is inserted through the mouth into the esophagus, stomach, and upper part of the small intestine allowing the doctor to see any inflammation or irritation. Endoscopy is performed under general anesthesia.
- Technetium gastric emptying study: The child is given milk or food mixed with a very weak radioactive chemical called technetium. The technetium is then followed through the gastrointestinal tract with a special camera to determine where the milk or food ends up and for how long. This procedure can detect if a patient’s stomach is emptying too slowly.
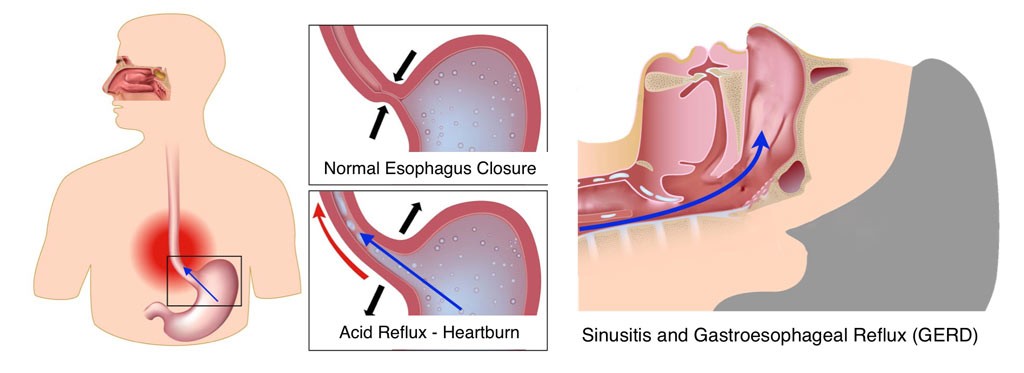
Laryngopharyngeal Reflux
Treating Gastroesophageal Reflux Disease (GERD) in Children
If your child is an infant, treatment will generally be focused on lessening symptoms, as the underlying problem typically resolves itself in time. Some successful measures used to reduce symptoms are:
- Elevating the head of the child’s crib
- Thickening the baby’s milk or formula with rice cereal or thickening agents (only with doctor’s recommendation)
- Holding the baby upright after feedings for 30 minutes
- Introducing solid foods (only with doctor recommendation)
Treatment for older children experiencing GERD includes similar measures, as well as lifestyle and dietary changes and possibly medication. Common treatments include:
- Raising the head of the child’s bed
- Eating small, more frequent meals instead of 3 larger meals per day
- Remaining upright for 2-3 hours after eating
- Regular exercise
- Avoiding foods that may aggravate symptoms, such as carbonated beverages, citrus, caffeine, chocolate, fried or spicy foods
- Medication: Your doctor may prescribe a medication for your child or recommend an over-the-counter medicine in order to decrease intestinal gas, or neutralize stomach acid. Consult your doctor before giving your child any over-the-counter medications for GERD.
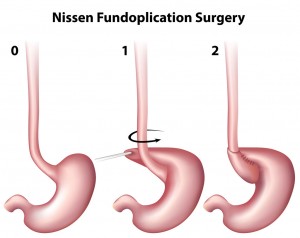 In extremely rare cases, a child may require antireflux surgery (Nissen Fundoplication) to correct GERD when symptoms do not respond to medical therapy. The anti-reflux surgery tightens the muscles at the bottom of the food pipe (esophagus), the tube that carries food from the mouth to the stomach. In this surgical procedure the surgeon will use stitches to wrap the upper part of your child’s stomach around the end of the esophagus. This helps prevent stomach acid and food from flowing back up.
In extremely rare cases, a child may require antireflux surgery (Nissen Fundoplication) to correct GERD when symptoms do not respond to medical therapy. The anti-reflux surgery tightens the muscles at the bottom of the food pipe (esophagus), the tube that carries food from the mouth to the stomach. In this surgical procedure the surgeon will use stitches to wrap the upper part of your child’s stomach around the end of the esophagus. This helps prevent stomach acid and food from flowing back up.
If you are concerned that your child may have GERD or is experiencing symptoms of GERD, please set up an appointment with our office.
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact Dr. Mona Dave’s Frisco Office.
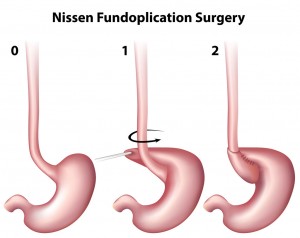 In extremely rare cases, a child may require antireflux surgery (Nissen Fundoplication) to correct GERD when symptoms do not respond to medical therapy. The anti-reflux surgery tightens the muscles at the bottom of the food pipe (esophagus), the tube that carries food from the mouth to the stomach. In this surgical procedure the surgeon will use stitches to wrap the upper part of your child’s stomach around the end of the esophagus. This helps prevent stomach acid and food from flowing back up.
In extremely rare cases, a child may require antireflux surgery (Nissen Fundoplication) to correct GERD when symptoms do not respond to medical therapy. The anti-reflux surgery tightens the muscles at the bottom of the food pipe (esophagus), the tube that carries food from the mouth to the stomach. In this surgical procedure the surgeon will use stitches to wrap the upper part of your child’s stomach around the end of the esophagus. This helps prevent stomach acid and food from flowing back up.