20 Jul Ulcerative Colitis (UC)
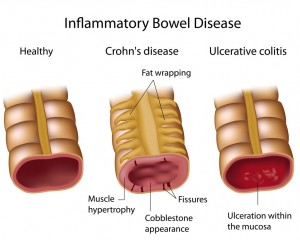
Ulcerative colitis (UC) is an inflammatory bowel disease (IBD) in which the lining of the large intestine (colon) becomes inflamed and sores called ulcers develop which produce mucus and pus. Ulcerative colitis occurs when the body’s immune system mistakes food and other necessary materials in the intestine for invading substances. The immune system then sends white blood cells into the intestinal lining causing inflammation and ulcerations.
Ulcerative colitis is different from Crohn’s disease in that UC affects the colon and the lining of the colon while Crohn’s can affect any part of the gastrointestinal (GI) tract and all layers of the bowel wall.
Symptoms of Ulcerative Colitis in Children
Symptoms of ulcerative colitis typically develop over time, but can appear suddenly and progress quickly in some cases. Your child may experience symptoms ranging from mild to severe without any obvious reason. Symptoms of ulcerative colitis include:
- Frequent diarrhea, often with pus or blood
- Abdominal cramping and pain
- Urgent need to have a bowel movement
- Rectal pain and bleeding
- Fever
- Unexplained fatigue
- Loss of appetite
- Weight loss
- Anemia or low iron level
- Eye, joint, or skin irritations
- Growth or developmental delay
Children with ulcerative colitis tend to have time periods where symptoms subside and then later flare up. These remission periods can last months or even years, but symptoms do return eventually.
Causes of Ulcerative Colitis in Children
Ulcerative colitis does not have a known cause, however research suggests a combination of factors:
Heredity: Children whose parents have IBD are more likely to have ulcerative colitis.
Immune System: Researchers believe a malfunctioning immune system damages the intestine.
Environment: Environmental antigens may be a direct cause or a stimulant to the immune system.
Many scientists believe that patients with UC have an abnormal interaction between an infection and the body’s immune system. In this process, inflammation, which is normally produced temporarily to fight the infection, continues even after the infection has cleared. Approximately 1.4 million Americans are affected by inflammatory bowel disease, with 100,000 being children. Risk factors for UC include:
Ethnicity: Caucasians have the highest risk, especially those of Ashkenazi Jewish heritage.
Age: UC typically starts before age 30, but can present at any age.
Family History: Children who have a parent or other close relative with UC are at higher risk.
Use of Isotretinoin: A medication used to treat acne that may contribute to UC.
Complications of Ulcerative Colitis in Children
Complications of ulcerative colitis can arise not only from the condition itself, but also from insufficient nutritional intake. Children with UC can have difficulty getting and absorbing enough calories for proper development. Complications may include:
- Nutritional deficiency
- Delayed development
- Severe bleeding
- Perforated colon
- Rapid swelling of the colon (toxic megacolon)
- Dehydration
- Mouth sores
- Skin, joint, or eye problems
- Osteoporosis (bone loss)
- Anemia
- Increased risk of blot clots, colon cancer, and liver disease
Diagnosing Ulcerative Colitis in Children
Ulcerative colitis symptoms can vary depending on the age of your child and the location and severity of inflammation. Your doctor will likely want to collect extensive information about your child, so being well prepared for your appointment will ensure that it goes smoothly. Helpful steps you can take include:
- Keep a record of symptoms your child is experiencing, how often, and when they improve or worsen.
- Write down any changes or stresses in your child’s life.
- Bring a list of any medications your child takes.
- Be sure to follow any pre-appointment restrictions, such as fasting. If you are unsure, please ask our office staff if your child has any restrictions to follow.
- Write down any questions you have for the doctor.
- Bring a friend or relative: If you feel that having an additional person present will be helpful in remembering instructions or other information, please feel free to bring someone with you.
At your appointment, your doctor will perform a thorough examination and review your child’s medical history. Diagnostic testing to confirm a diagnosis may include:
- Blood test: To check for anemia, infection, or high white blood cell count.
- Stool sample: To check for blood, inflammation, or infection in the colon or rectum.
- X-rays: To locate the disease and check for complications.
- Upper GI Endoscopy – EGD: An ultra-thin, flexible tube equipped with lights and camera (endoscope) is inserted through the mouth into the esophagus, stomach, and upper part of the small intestine allowing the doctor to see inside the areas of the intestine. Tissue samples (biopsies) are taken to make a diagnosis. Endoscopy is usually performed under general anesthesia.
- Lower GI Endoscopy – Colonoscopy: A thin, flexible, long tube, equipped with a small light and camera, is inserted into the anus to examine the inside of the large intestine. Tissue samples (biopsies) are taken to make a diagnosis. Colonoscopy is performed under general anesthesia.
- CT scan: An abdominal or pelvic scan used to determine the extent of inflammation or if a complication exists.
The type of ulcerative colitis diagnosed depends on how much of your child’s colon is affected. The condition can range from mild to severe:
Ulcerative proctitis: The mildest type of ulcerative colitis in which inflammation is limited to the rectum, usually less than 6 inches.
Distal colitis (left sided): Areas of inflammation include the rectum extending as far as the splenic flexure (a sharp bend in the colon near the spleen).
Proctosigmoiditis: Areas of inflammation include the rectum and sigmoid colon (the portion of the colon just above the rectum).
Pancolitis: The entire colon is affected by inflammation.
Treating Ulcerative Colitis in Children
Treating ulcerative colitis involves regulating the immune system in order to control symptoms. With a proper combination of therapies, children with UC can experience a great reduction in symptoms and often long term remission. Goals of UC treatment:
- Controlling inflammation
- Relieving symptoms
- Correcting deficiencies in nutrition
Treatment will depend on what type of UC your child is diagnosed with and how severe the symptoms are. The type of ulcerative colitis diagnosed depends on how much of your child’s colon is affected. The condition can range from mild to severe. Medications that have been successfully used to treat symptoms are:
- Anti-inflammatory drugs: To treat localized inflammation.
- Immunomodulators: To suppress the immune system’s response to reduce inflammation.
- Antibiotics: To control or prevent infection.
- Biologic therapies: Treatment involves using antibodies to interfere with the disease’s inflammatory process.
Other treatments include:
- Nutritional counseling: Maintaining a healthy diet is vital for your child’s continued growth and development.
- Surgery: In severe cases or when complications arise, surgery may be required.
Home and Lifestyle Remedies for Ulcerative Colitis in Children
If your child is diagnosed with ulcerative colitis, you can make dietary and other lifestyle adjustments to help alleviate symptoms:
- Avoid foods which worsen symptoms: Keeping a food diary can help identify when symptoms arise and in conjunction with what foods.
- Drink plenty of water.
- Avoid caffeine.
- Use multivitamins: Getting proper nutrition can be challenging, so vitamin supplements can help maintain health.
- Exercise: Reducing stress and depression through exercise can help normalize bowel function.
- Probiotics: Live bacteria similar to the natural bacteria in the GI tract that come in tablet, pill, or powder form. Your doctor can advise you on the proper amount to improve UC symptoms.
- Educational Resources on Inflammatory Bowel Disease (IBD): Crohn’s and Colitis Foundation of America
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact us here.